Trauma team “goes to the wall” to improve loop closure – Trauma System News
Effective performance improvement (PI) requires an effective system for providing feedback to nursing staff and closing the loop on PI issues. That requires not just effective communication but a culture of accountability and engagement.
At Baylor Scott & White Medical Center – Taylor, a Level IV trauma center in Taylor, Texas, trauma program leaders and frontline staff collaborated to create an efficient and well accepted system for closing the PI loop. According to Gay Kurtz, their newly hired trauma program manager (TPM), this system has helped establish a culture of transparency, communication, mutual respect and accountability.
Challenge: Staff response to PI-related feedback
“My initial deep dive into the trauma program revealed a need to educate frontline staff on trauma standards and their personal role in the trauma process. Also, similar to many trauma centers, improvement was needed to the staff response to PI-related feedback to support improvement in trauma metrics. Staff needed to better understand trauma standards and take greater ownership of the entire trauma process, so changing the culture was critical.”
Innovation: Trauma Mailbox and Trauma Whiteboard
“My first priority as the newly hired TPM was to present a mandatory course for ED staff that covered trauma standards defined by ACS and the State of Texas. Next, a unit-based volunteer workgroup of frontline employees was created. Trauma standards, PIPS expectations and loop closure definitions were reviewed in detail with the workgroup members. Members were then asked how they wanted to receive required trauma PI feedback. The workgroup chose to create a Trauma Wall, situated near the staff entrance, that included a dedicated Trauma Mailbox and a Trauma Whiteboard.”
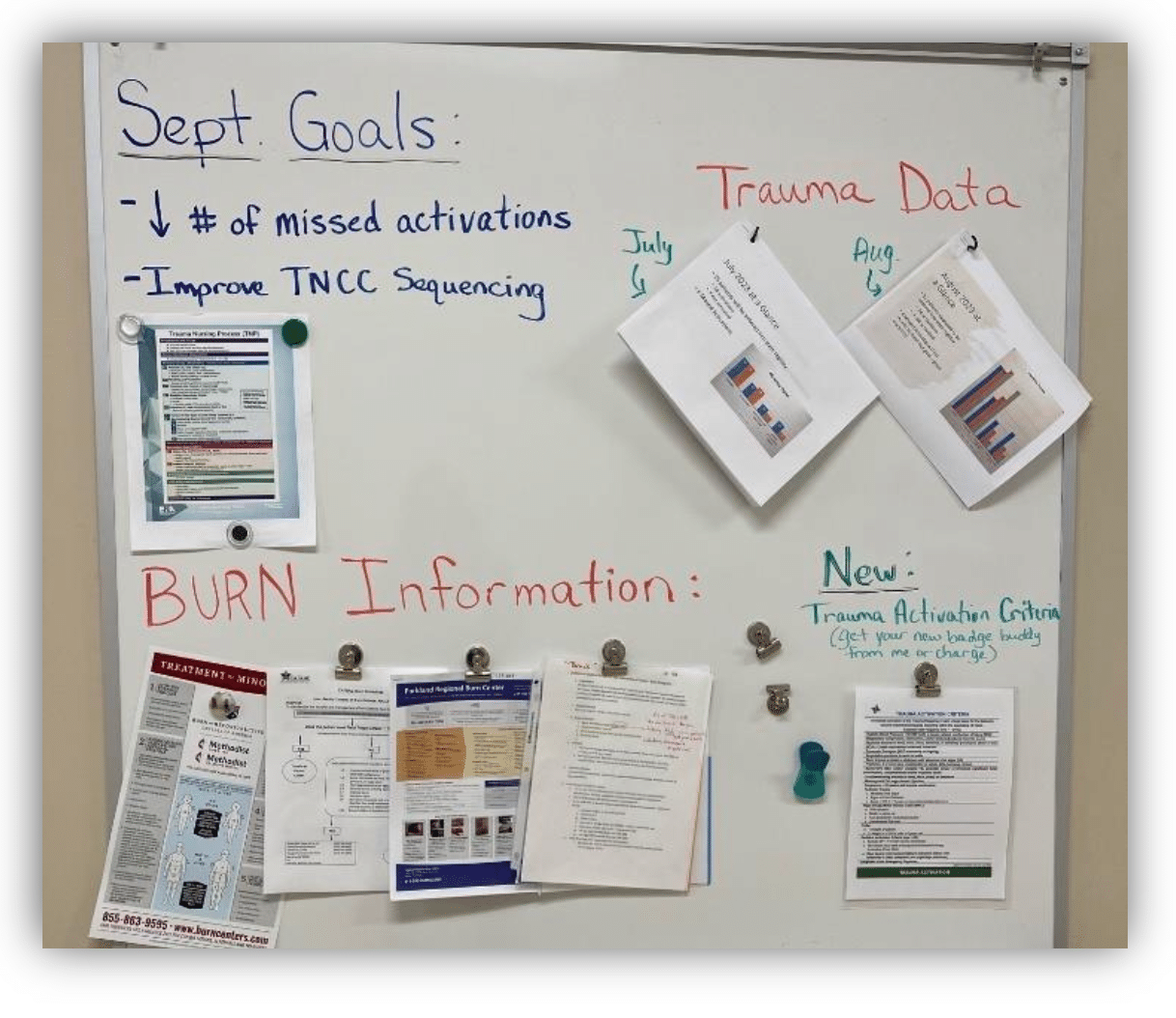
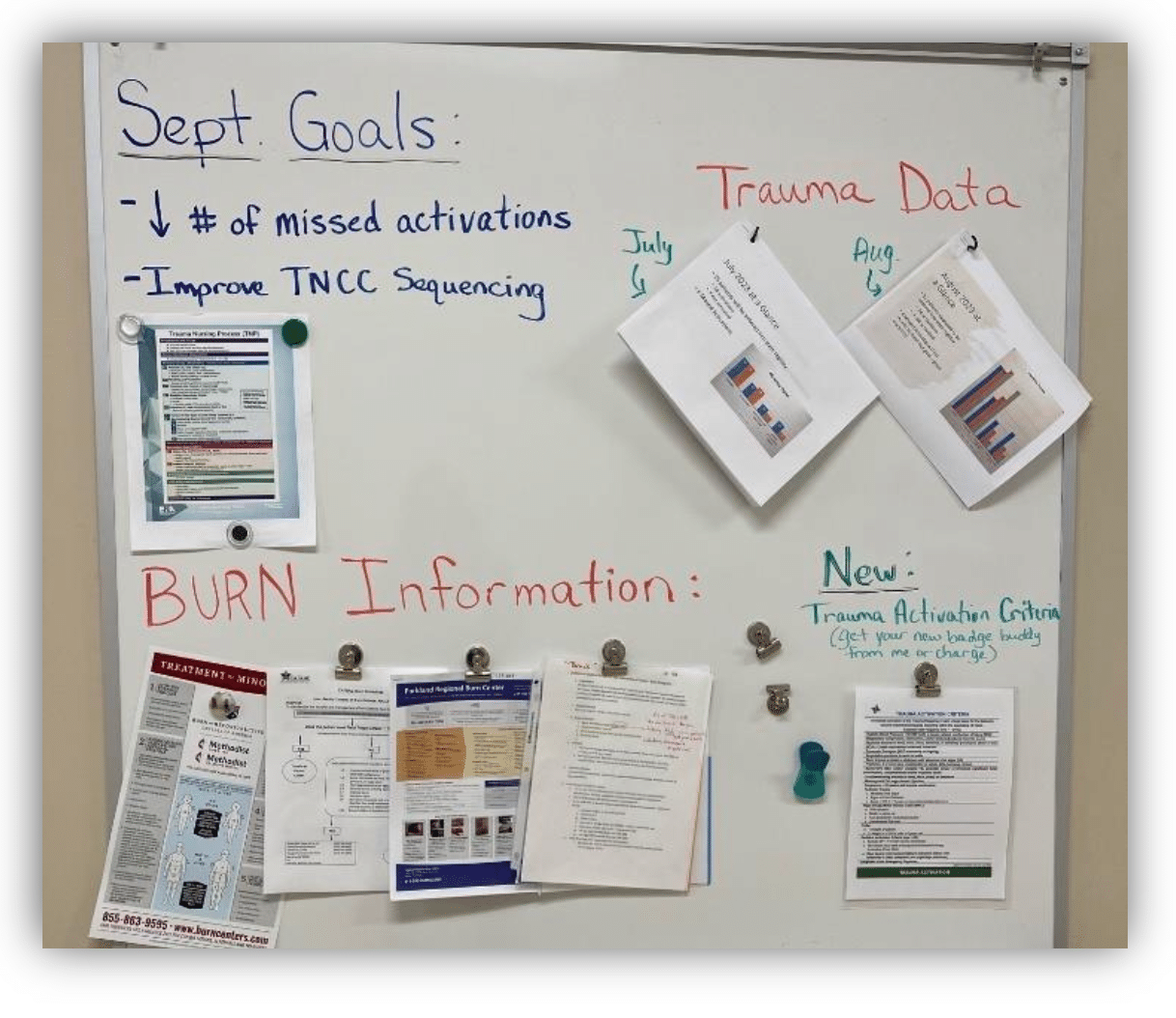
“The Trauma Whiteboard displays the PI topic of the month, shows monthly data trends and provides general education/announcements.”


“The Trauma Mailbox consist of a simple hanging folder system. Each staff member has their name on a slot, and each slot contains a green folder where feedback forms are placed. Staff receive feedback forms on all their trauma patients, including both OFIs and perfect trauma charts. If a form notes a deficiency (e.g., incomplete initial VS), the standard related to the deficiency is provided for education and staff are required to sign next to the identified deficiency. When staff come on duty, they check their folder for a feedback form, review the findings, sign it and return it to the TPM via her mailbox. The TPM monitors all findings and progress toward loop closure goals. The visible and formal nature of the mailbox (along with the required staff signature) creates a sense of accountability. This saves time as the new system doesn’t require constant follow-up, repeated emails and numerous meetings about and with staff.”
Results: Standards compliance and process improvement
“The new Trauma Wall created a unique opportunity to communicate deficiencies while simultaneously increasing education, accountability and loop closure. Coupled with signature-required feedback forms, it allowed us to meet the state’s PI standards and improve many trauma processes. In four months, we went from a <10% ‘staff acknowledged deficiencies’ rate to 100% acknowledgment. We also decreased ‘Missed Trauma Activations’ from 40% in June 2023 to 0% missed activations by December 2023. The Trauma Wall has also proven effective at closing numerous PI topics related to nursing documentation (i.e., documentation of MD arrival, VS, I&Os, ESI Levels, Trauma Flowsheet, etc.). It has been amazing to see the staff learn, be open to feedback, and respond with improved compliance.”



